How Much Does an EMR Cost in 2025? Complete Pricing Guide
- Pritesh Sonu

- Jul 6
- 8 min read
It’s mid-2025. You walk into a clinic with no clipboards, no paperwork. In just a tap, your doctor accesses your full medical history, checks for allergy alerts, updates your prescription, and sends your lab order, all in a matter of seconds. That’s the magic of an EMR (Electronic Medical Record).
But here’s the catch: Setting up an EMR isn’t a plug-and-play process. Behind that effortless experience lies a complex world of costs, including licenses, hardware, training, data migration, compliance steps, and support. Curious about what it really takes to implement one? Let’s break down those costs, in simple terms, and see what you can expect in 2025.
What is an EMR?
An Electronic Medical Record (EMR) is just a digital version of the old paper chart. It holds everything: your medical history, test results, prescriptions, and even appointment notes. That means no lost files, faster care, and fewer mistakes.
Key features include:
Digital charts that make information easy to find
Scheduling tools with reminders
E‑prescribing and labs are sent automatically.
Simple reports and dashboards showing patient trends
Strong data protection to comply with laws like HIPAA
All of this helps doctors work faster, avoid errors, and treat patients more safely.
EMR vs. EHR: What’s the Difference?
You might hear EMR and EHR used interchangeably, but they serve slightly different purposes:
An EMR (Electronic Medical Record) is a digital version of the paper charts used within a single clinic or hospital. Picture it as a secure digital notebook that stores patient histories, prescriptions, lab results, and visit notes, all within one facility. It’s perfect for tracking visits, prescriptions, lab orders, and day-to-day patient notes. However, its focus remains within one facility; it doesn’t easily share data with others.
On the other hand, an EHR (Electronic Health Record) is designed to be shared. Think of it as a cloud-connected system that integrates data across multiple healthcare providers, including clinics, hospitals, labs, specialists, and even pharmacies. It follows the patient across their entire care journey, enabling better collaboration and continuity. EHRs are designed for sharing, often utilizing interoperability standards like FHIR to ensure secure and seamless data exchange. In short:
EMR = internal use, limited sharing
EHR = broader scope, coordinated care
That said, the line between the two is becoming increasingly blurred. Many modern platforms now bundle EMR and EHR capabilities into a single solution, providing the best of both worlds.
Which One Should You Choose?
If your clinic operates solo or within a small team and doesn’t need to exchange records with outside providers, an EMR is often the smart, cost-effective choice. It offers everything needed for daily patient care—charting, e-prescriptions, scheduling—without unnecessary extras or heavy technology burdens.
However, if you’re part of a larger network or want to connect hospitals, labs, or specialists, an EHR becomes more sensible. The added investment pays off in long-term benefits, including integrated patient histories, smooth referrals, analytics, and compliance, making it ideal for organizations focused on growth.
What Influences the Cost of an EMR?

1. Size of Your Practice
Solo or small practice: You can expect a modest setup cost ($1,500–$5,000) and affordable monthly subscriptions ($200–$700 per provider).
Medium to large practices: More providers mean more licenses, more training, and more customization, which pushes initial costs to $20,000–$150,000 and higher monthly fees as well.
2. Deployment: Cloud vs. On-Premises
Cloud EMR: Lower upfront cost, includes hosting, maintenance, and automatic updates. You pay a steady monthly fee and skip the setup of a server room.
On-Premises EMR: You own the servers and software. Upfront costs can reach $1,200–$ 500 K+, plus you’ll need IT staff, hardware maintenance, and security checks.
3. Vendor & Features
Premium vendors like Epic or Cerner offer robust systems designed for large health systems, but come with a hefty price tag ($20K–$70K/provider upfront)
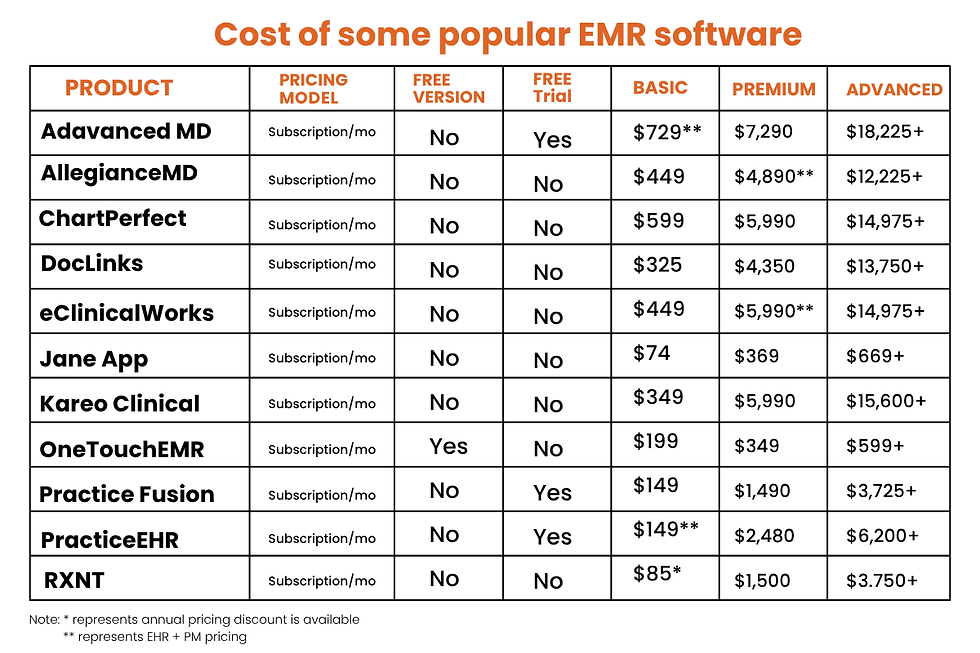
Mid-range players, such as Athenahealth or eClinicalWorks, charge $140–$700 per month per provider. They balance features and cost.
Budget-friendly systems (e.g., DocVilla, Practice Fusion) typically range from $100 to $300 per month per provider, making them ideal for small practices.
4. Implementation & Training
Setting up the system and teaching staff how to use it is crucial. Small clinics may budget $1,000–$5,000, but larger facilities might spend $20,000–$100,000 or more, depending on workflow customization and data import needs.
5. Data Migration & Testing
Moving patients’ records, whether paper or old digital files, requires time and care. Test runs are needed to ensure accuracy. Practice size determines the cost, but setups range from $2,000 to $50,000, and comprehensive testing may add several thousand more.
6. Compliance & Security
Depending on local laws and standards (like HIPAA in the U.S.), you’ll need encryption, secure backup systems, staff training, and regular audits. Initial setup may cost $5,000–$50,000, with ongoing compliance checks adding recurring expenses.
Real-World Perspective:
A Reddit user setting up a physical therapy clinic found DocVilla to be charged around $100–$350 per month per provider and praised its customizable features, unlike cheaper systems that later require multiple add-ons.
Another user paid $1,000–$1,500 per month for Fusion EMR across eight users; switching to a simpler system, such as Carepatron, saved them significantly while still meeting their needs.
These stories show how practice size, feature needs, and vendor choice directly affect costs and satisfaction.
Real-World Cost Ranges (2025 Data):
According to RevenueXL, typical costs in 2025 include:
Solo/small practice:
Setup: $1,500–$5,000
Monthly: $200–$700/provider
Medium-sized practice:
Setup: $20,000–$100,000+
Monthly: $500–$2,000+
Large hospitals:
Setup: $250,000–$ 1 M+
Monthly: $10,000–$35,000+
A Tech Web source chart from Sparx estimates:
Solo clinic (1–3 providers): $15K–$30K initial; $4.7K–$9.1K yearly
Small practice (4–10 providers): $54K–$111K initial; $20K–$66K yearly
Small hospital (<100 beds): $170K–$400K initial; $57K–$99K yearly
How EMRs Deliver ROI:
1. Financial Break-even in Under a Year for Clinics
Many primary care clinics break even in 10–12 months after EMR implementation. Research on 17 U.S. primary-care sites found an average recovery time of 10 months, driven by improved efficiency: 27% more patients seen per clinician and 10% more active patients overall. Clinics often generate $4,000–$7,000 additional net revenue per provider each month, primarily due to improved documentation and optimized billing.
2. Major Cost Reductions in Hospitals
In larger systems, EMRs deliver savings in hospital length-of-stay, lab testing, transcription, and staffing:
A U.S. inpatient study showed 18% fewer lab tests, a 74% decrease in transcription costs, and a 10–14% drop in medication errors soon after EMR went live.
At Samsung Medical Center (South Korea), the EMR rollout resulted in increased bookings and efficiencies over an eight-year period, yielding a net present value (NPV)of $3.6 million, a benefit-cost ratio of 1.23, and a payback period of 6.2 years.
3. Massive Long-Term System Savings
Top U.S. health systems report multi-billion-dollar benefits:
Stanford Medicine: saved about $1 billion over 10 years
Kaiser Permanente realized $1.7 billion in savings.
Intermountain Healthcare: Avoided $2 billion in costs.
The Mayo Clinic reported $1.5 billion in improvements in care and efficiency.
Therefore, in 2025, EMRs will provide ROI in three phases:
Clinics break even in ~10–12 months through productivity and billing improvements.
Hospitals achieve cost reductions in lab use, transcription, and length of stay, paying off in ~3–6 years.
Large health systems accrue multi-billion-dollar benefits over a decade.
The message is clear: while EMRs require upfront investment, they pay back quickly for clinics and offer immense long-term savings for hospitals and integrated health systems.
Licensing and Subscription Fees (Cloud‑based EMR)
Cloud-based EMRs are typically billed monthly per provider. Your monthly subscription depends on the number of users, included features, and the amount of data storage.
Starting point: Around $200/month for small clinics needing basic charting, scheduling, and simple reporting.
Advanced features: Up to $1,500/month if you need telemedicine, analytics, patient portals, or EHR interoperability.
User count matters: More providers or staff increase your bill—each user counts toward licensing costs.
Budget tip: Always check what’s included—some vendors charge extra for add-ons like lab integration or compliance support.
Initial Setup and Configuration Costs
This covers preparing the system for clinical use, including installing software, configuring workflows, and integrating basic tools.
Smaller practices: Typically $10,000–$50,000, depending on the level of customization.
Multi-site clinics: Expect the upper end—more workflows and departments to map.
What it includes: Implementation fees cover vendor-led configuration and basic integrations, such as scheduling or e-prescribing.
Why does it matter? Proper setup ensures the system aligns with your day-to-day work, minimizing frustration and downtime.
Integration Costs (Linking Systems Together)
To function smoothly, EMRs often need to integrate with existing software, such as lab systems, billing systems, or radiology tools.
Basic integration: Around $5,000 for light connections (e.g., to a scheduler or e-prescribing tool.
Complex integration: $50,000–$100,000+ for hospital-level integrations (labs, imaging, billing).
APIs and testing: Includes developer hours, security checks, and real-time data syncing.
Tip: Identify must-have links upfront; adding them later can be more costly.
Training and Onboarding:
Your staff needs to learn how to use the new system, which involves training sessions, practice time, and ongoing support.
Small teams: $1,000–$5,000 total, depending on the number of users and training depth.
Large practices can incur costs of tens of thousands, especially with role-based training for doctors, nurses, and front desk staff.
What it covers: Hands-on vendor sessions, workflow familiarization, and help desk during go-live.
Why it matters: Under-trained staff slow down the clinic and may make errors—training pays off.
Data Migration and Testing:
Moving patient records from paper or old systems into the EMR, followed by rigorous checks to ensure data and workflows function properly.
Migration cost: $2,000–$50,000, depending on the amount and complexity of data.
Testing and QA: Typically $10,000–$50,000 to validate workflows, user panels, and compliance.
Why both are essential: Bad data or untested workflows can cause clinical mistakes or billing errors.
Pro tip- Ask vendors for a sandbox version for testing before going live.
Closing Thoughts
Investing in an EMR in 2025 means more than buying software. It means transforming how care is delivered. Yes, there are costs involved, from licenses and setup to training and support, but with the right planning (and the right partner), those costs can turn into serious value in just a few years.
Let’s be honest: in today’s tech-driven world, EMRs aren’t optional anymore; they’re essential. But when you get it right, you’re not just ticking a box. You’re making your practice more efficient, more secure, and way more patient-friendly. So if you're thinking about making the move, now’s the time. Plan smart, budget wisely, and select a solution that evolves with you. The payoff? A smoother practice, happier patients, and a future-ready clinic. Sounds worth it, doesn’t it?
Faqs
1. What is an EMR and how does it work in a clinic?
An EMR, or Electronic Medical Record, is a digital version of a patient’s paper chart. It stores medical history, test results, prescriptions, and appointment notes, making information easy to access and update for healthcare providers.
2. How much does it cost to implement an EMR system in 2025?
In 2025, EMR implementation costs vary by practice size and features. Small clinics can expect setup costs of $1,500–$5,000 and monthly fees of $200–$700 per provider. Medium practices may spend $20,000–$100,000+ upfront, while large hospitals can see costs from $250,000 to over $1 million.
3. What are the main factors that influence EMR costs?
Key cost drivers include practice size, deployment type (cloud vs. on-premises), vendor choice, features, integration needs, training, data migration, and compliance requirements.
4. What is the difference between EMR and EHR?
An EMR is used mainly within a single clinic or hospital, while an EHR (Electronic Health Record) is designed for sharing patient data across multiple providers and healthcare settings.
5. Are there hidden costs when setting up an EMR?
Yes, hidden costs can include training, data migration, system integration, ongoing support, compliance upgrades, and productivity loss during setup.
6. How do cloud-based EMR costs compare to on-premises systems?
Cloud-based EMRs have lower upfront costs and are billed monthly, typically $200–$700 per provider. On-premises systems require a larger initial investment but may have lower long-term subscription fees.
7. How long does it take for a clinic to see ROI from an EMR investment?
Most clinics break even within 10–12 months due to improved efficiency and billing. Hospitals and large systems may see major savings in 3–6 years, with long-term benefits in the billions for large networks.
8. What are the ongoing costs for EMR maintenance and support?
Ongoing costs include monthly subscription fees, software updates, technical support, compliance checks, and periodic staff training. These can range from $10,000 to $100,000 per year for larger organizations.
9. Can EMRs help reduce costs and improve care quality?
Yes, EMRs help reduce errors, streamline workflows, and optimize billing, leading to significant cost savings and better patient outcomes over time.
10. What should I consider when choosing an EMR vendor in 2025?
Consider your practice size, required features, integration needs, compliance standards, training and support options, and total cost of ownership before selecting a vendor.



Comments